The Centers for Disease Control and Prevention (CDC) report that the COVID-19 variant first identified in the U.K.—B.1.1.7—is the most common cause of new infection in the U.S, particularly in Florida, Michigan, Minnesota, Massachusetts, Colorado, California, Maryland, Pennsylvania, and New Jersey.1 This strain has evidence of being more infectious and causing more severe disease compared with the original strain.2 Other variants of concern circulating in the U.S. are P.1 and B.1.351, first identified in Brazil and South Africa, respectively, and B.1.427 and B.1.429 which were first identified in California.3
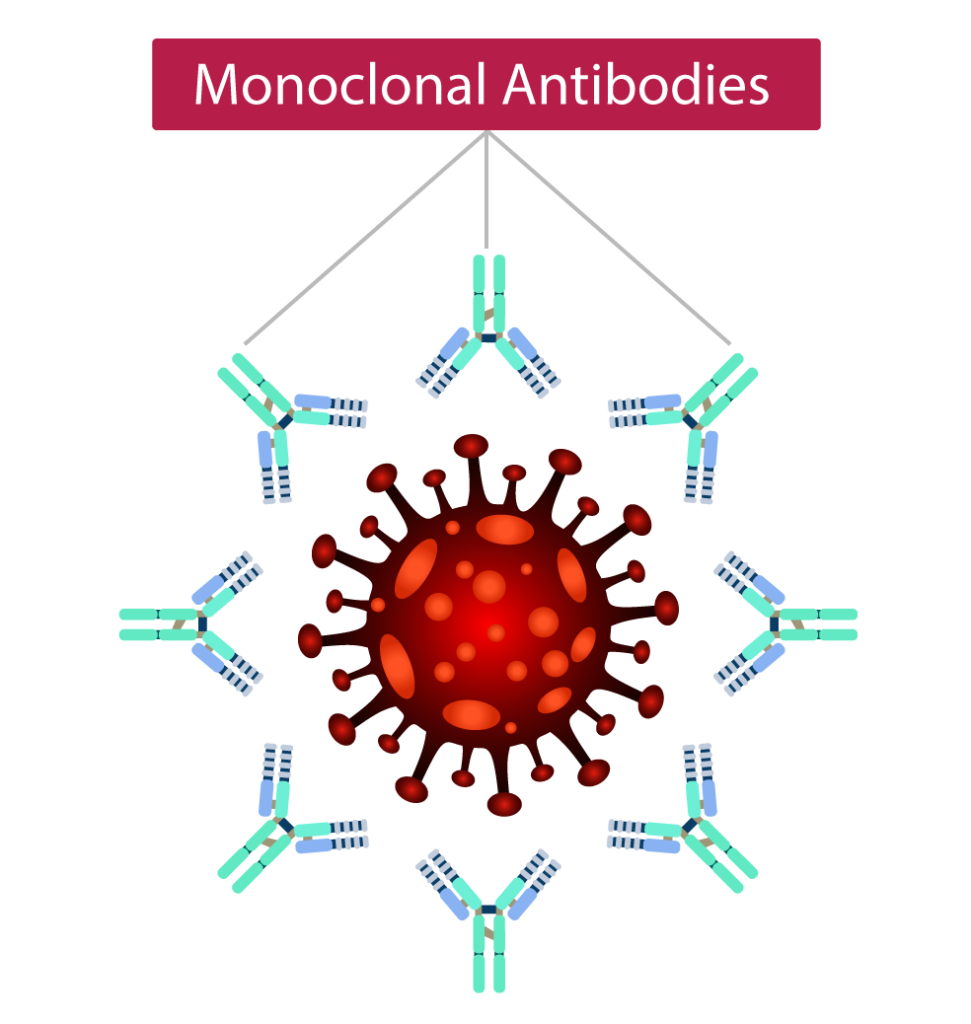
Monoclonal antibodies (mAbs) and mAb cocktails that have received Emergency Use Authorization (EUA) by the US Food and Drug Administration (FDA) have shown efficacy in preventing mild-to- moderate COVID-19 from progressing to severe disease in people with certain risk factors.4–6 Because of concern that single-agent mAbs are ineffective against the variants, the distribution of bamlanivimab (LY-CoV555) as monotherapy was halted nationwide.7
Preclinical data of bamlanivimab with etesevimab (LY-CoV016/JS016) show that this combination continues to remain effective against the B.1.1.7 variant but has reduced activity against the B.1.351 variant; it continues to be available based on its EUA.8,9
Unpublished data from a phase 3 trial of 4567 high-risk non-hospitalized people with COVID-19 show that the mAb cocktail consisting of casirivimab with imdevimab (REGN-COV™) reduced hospitalizations or death by 70% and significantly reduced symptom duration by 4 days compared with placebo. All doses of the antibody cocktail—8000 mg, 2400 mg, and 1200 mg—showed similar efficacy.10 A companion dose-ranging phase 2 trial of 803 non-hospitalized people with COVID-19 showed significant and comparable viral reductions for all REGEN-COV doses tested, including as low as 300 mg.10 The FDA recently updated U.S. EUA fact sheets for all authorized monoclonal antibody treatments, indicating that compared with other mAbs, REGEN-COV retains potency against several key variants of concern circulating in the U.S.8,11
REGEN-COV continues to be investigated on ongoing clinical trials in both the outpatient and hospital settings.
References
- Centers for Disease Control and Prevention (CDC). US COVID-19 cases caused by variants. Updated 4/6/2021. (www.cdc.gov/coronavirus/2019-ncov/transmission/variant-cases.html) Accessed 4/8/2021.
- Davies NG, Abbott S, Barnard RC, et al. Estimated transmissibility and impact of SARS-CoV-2 lineage B.1.1.7 in England. Science. 2021;March 3: Epub ahead of print.
- CDC. SARS-CoV-2 Variant classifications and definitions. Updated 3/16/2021. (www.cdc.gov/coronavirus/2019-ncov/cases-updates/variant-surveillance/variant-info.html#Concern) Accessed 4/8/2021.
- Weinreich DM, Sivapalasingam S, Norton T, et al. REGN-COV2, a neutralizing antibody cocktail in outpatients with COVID-19. N Engl J Med. 2021;384:238-251.
- Chen P, Nirula A, Heller B, et al. SARS-CoV-2 neutralizing antibody LY-CoV555 in outpatients with Covid-19. N Engl J Med. 2021;384:229-237.
- Gottlieb RL, Nirula A, Chen P, et al. Effect of bamlanivimab as monotherapy or in combination with etesevimab on viral load in patients with mild to moderate COVID-19: a randomized clinical trial. JAMA. 2021;325:632-644.
- Department of Health and Human Services (DHHS). Outpatient monoclonal antibody treatment for COVID-19 made available under emergency use authorization. (www.phe.gov/emergency/events/COVID19/investigationMCM/Bamlanivimab/Pages/default.aspx) Accessed 4/8/2021.
- US Food and Drug Administration (FDA). Fact sheet for health care providers: Emergency Use Authorization (EUA) of bamlanivimab and etesevimab. Updated 3/2021. (www.fda.gov/media/145802/download). Accessed 4/8/2021.
- Wang P, Nair JS, Liu L, et al. Antibody resistance of SARS-CoV-2 variants B.1.351 and B.1.1.7. Nature. 2021;Mar 8: Epub ahead of print.
- Regeneron press release. Phase 3 trial shows REGEN-COV™ (casirivimab with imdevimab) antibody cocktail reduced hospitalization or death by 70% in non-hospitalized COVID-19 patients. (https://investor.regeneron.com/node/24986/pdf) Accessed 4/8/2021.
- FDA. Fact sheet for health care providers Emergency Use Authorization (EUA) of REGEN-COV (casirivimab with imdevimab). Updated 3/2021. (www.fda.gov/media/145611/download) Accessed 4/8/2021.